Deep vein thrombosis, or DVT, is a blood clot that forms in a vein deep in the body, usually in the lower leg or thigh. A DVT can become dangerous or even life-threatening if it breaks loose and travels to the lung, called a pulmonary embolism. Learning the signs of blood clots and ways to prevent them can help protect you from this serious health problem, says Sean Wengerter, MD, a vascular surgeon at Rockland Thoracic & Vascular Associates, PC, in Pomona, NY.
Who Gets DVTs?
“Patients who have had surgery, particularly to the hip or knee, are often at risk of DVT,” said Dr. Wengerter. “That’s because inflammatory factors are released by the body after surgery, which increases the risk of clotting.”
Other common risk factors include:
- Severe trauma, such as a car accident
- Injury to a vein that may have been caused by a broken bone or severe muscle injury
- Cancer and cancer treatments
- Pregnancy, which includes up to three months after the baby is born
- The use of hormone therapy that contains estrogen
- A family history of blood clots
- Obesity
- Confinement to bed
- Sitting too long, especially with legs crossed
Talk to your doctor if you have any of these risk factors.
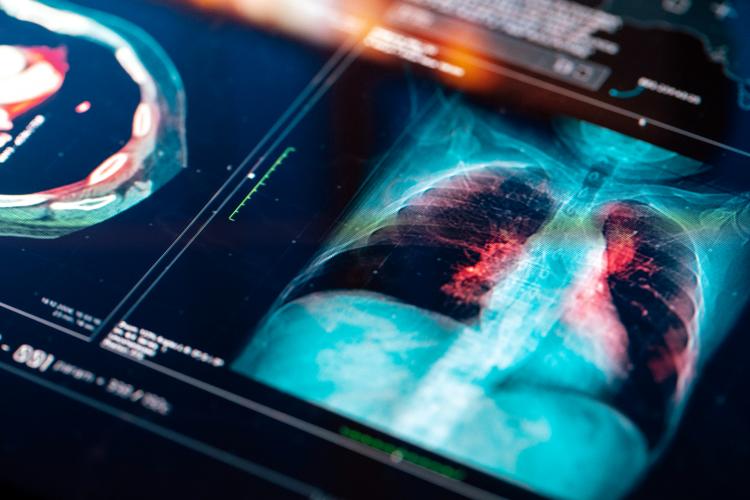
Diagnosing a DVT
Signs of a DVT include:
- Swelling, usually in one leg (or arm)
- Leg pain or tenderness often described as a cramp or Charley horse
- Reddish or bluish skin discoloration
- Leg (or arm) warm to touch
The doctor may order an ultrasound or MRI to diagnose a DVT.
Treatment
“Blood thinners such as heparin or warfarin are the gold standard treatment,” Dr. Wengerter said.
These medications slow the body’s ability to form new clots and keep existing clots from getting bigger. Many patients take blood thinners for weeks, months, or even years to prevent clots from returning.
For patients who cannot take blood thinners, the doctor may recommend that a filter be implanted in the large vein in the abdomen that brings blood from the lower body back to the heart. The filter prevents a clot from traveling from the leg or arm to the lung. A person can’t take blood thinners if they will be having major surgery in the near future, or if they recently had surgery such as a hip replacement. In those cases, the filter is implanted, and then removed once the patient can start taking blood thinners.
Preventing DVT
To prevent a DVT, get up and move if you’ve been sitting for a long time or traveling for an extended period by plane, train or car. “Stand up, walk around and flex your calves every two to three hours,” Dr. Wengerter said. If you have a history of clots or leg swelling, your doctor may recommend you wear compression stockings, which can help circulation by preventing blood from pooling in the veins.
If you are having orthopedic surgery, your risk for developing DVT is highest from 2 to 10 days after surgery. You remain at risk for about three months. Talk to your doctor about ways to prevent DVT before and after you have surgery. The doctor may prescribe medication, exercise and compression stockings. “In recent years, we have become very aggressive with giving surgery patients anti-clotting drugs called anticoagulants to prevent blood clots,” Dr. Wengerter said.
It is also important to know the signs of a pulmonary embolism, which require an immediate trip to the ER:
- Sudden shortness of breath
- Chest pain-sharp, stabbing; may get worse with deep breath
- Rapid heart rate
- Unexplained cough, sometimes with bloody mucus
“Blood clots are preventable and can be safely treated,” Dr. Wengerter said. “Learning the signs of blood clots and pulmonary embolism can save your life or the life of someone else.”


 Upcoming Events
Upcoming Events